Will Increasing Testosterone Reduce Gynecomastia?


Key Takeaways
- Increasing testosterone can reduce gynecomastia when low testosterone levels cause the condition, but may worsen it if testosterone converts to estrogen through aromatization.
- The effectiveness depends on the underlying cause of gynecomastia and individual hormone metabolism patterns.
- Testosterone replacement therapy requires careful monitoring and may need to be combined with aromatase inhibitors to prevent estrogen conversion.
- Chronic gynecomastia with established fibrous tissue may not respond to hormone therapy alone and could require surgical intervention.
- Medical supervision is essential when using testosterone therapy to treat gynecomastia, as improper dosing can worsen the condition
The answer to whether increasing testosterone reduces gynecomastia depends heavily on the underlying cause of breast tissue growth, individual hormone metabolism, and proper medical management. Understanding these factors is crucial before considering testosterone therapy as a gynecomastia treatment option. Men with gynecomastia may also experience anxiety or stress related to their appearance, which underscores the importance of addressing both physical and emotional aspects of the condition. The condition can be particularly challenging for adolescents, forming their self-identity. Gynecomastia can lead to low self-esteem and social withdrawal, further emphasizing the need for comprehensive care.
Many men struggling with gynecomastia wonder whether increasing testosterone could solve their breast enlargement problem. The relationship between testosterone levels and male breast tissue development is far more complex than initially appears. While testosterone therapy can help reduce gynecomastia in specific circumstances, it may actually worsen the condition in others. Gynecomastia is common during three life stages: in newborns, during puberty in adolescents, and in older adults over 60 years of age. Physiological gynecomastia in newborns is partly caused by high fetal blood levels of estradiol and progesterone from the mother.

The Complex Relationship Between Testosterone and Gynecomastia
The question of whether increasing testosterone will reduce gynecomastia doesn’t have a simple yes or no answer. Gynecomastia develops from an imbalance between estrogens, which stimulate breast tissue growth, and androgens like testosterone, which suppress male breast enlargement. Hormonal imbalance, particularly changes in the testosterone ratio and hormone changes during different life stages, can lead to gynecomastia.
This delicate hormone balance determines whether breast tissue proliferates or remains minimal. Estrogen levels increase in men with lower testosterone due to higher aromatase activity in adipose tissue. Additionally, conditions like thyrotoxicosis in males are linked to gynecomastia, possibly due to increased estrogen conversion and elevated LH levels. The adrenal glands also play a role in hormone production, and tumors or dysfunction in the adrenal glands can contribute to gynecomastia by altering hormone levels. In older men, gynecomastia prevalence ranges from 36 to 57% due to increased peripheral aromatase activity and decreased testosterone levels.
When testosterone levels are genuinely low, restoring them to normal ranges can help prevent further breast tissue growth and reduce existing enlargement in early-stage cases. Low testosterone can cause gynecomastia by reducing the suppression of breast tissue growth, a mechanism sometimes referred to as ‘testosterone cause gynecomastia.’ However, when testosterone levels are already adequate or when the body converts excess testosterone to estrogen through a process called aromatization, testosterone therapy can paradoxically worsen gynecomastia. Estrogen excess resulting from increased aromatization can contribute to gynecomastia.
The effectiveness of testosterone therapy for treating gynecomastia also depends on timing. Early-stage gynecomastia with active glandular tissue may respond better to hormonal interventions, while chronic gynecomastia with established fibrous tissue rarely improves with hormone therapy alone. Understanding individual hormone metabolism patterns becomes critical for predicting treatment success. Testosterone imbalance, such as a decrease in testosterone relative to estrogen, is a key factor in the development of gynecomastia.
How Testosterone Affects Male Breast Tissue

Testosterone plays a crucial role in maintaining the masculine chest contour by suppressing breast tissue development. In male breast tissue, testosterone binds to androgen receptors and counteracts estrogen’s growth-promoting effects. When testosterone levels drop below optimal ranges, this protective mechanism weakens, creating favorable conditions for developing gynecomastia.
The relationship between testosterone and male breast tissue involves complex feedback mechanisms. Testosterone not only directly suppresses breast tissue growth, but also influences the production and activity of other hormones that affect breast development. Low testosterone can lead to compensatory increases in other hormones, including those from the pituitary gland, which indirectly promotes breast tissue growth. The pituitary gland regulates gonadotropin secretion, which stimulates the testes to produce testosterone. Disruptions in gonadotropin secretion can impair testosterone synthesis, resulting in decreased testosterone levels and contributing to gynecomastia. Increased prolactin levels may inhibit gonadotropin-releasing hormone release, leading to secondary hypogonadism and gynecomastia. A combination of hormonal and external factors, such as medication use, anabolic steroids, or exposure to certain chemicals, causes gynecomastia by increasing estrogen levels or lowering testosterone.
Adrenal tumors can secrete excess hormone that may be aromatized to estrogen, contributing to gynecomastia.
Male breast tissue contains receptors for both androgens and estrogens, making it responsive to fluctuations in these hormones. When testosterone levels are insufficient to adequately activate androgen receptors, estrogen can dominate by binding to estrogen receptors, resulting in the proliferation of glandular breast tissue and the development of enlarged breast tissue. These hormonal imbalances can lead to abnormal breast growth in males.
Age-related testosterone decline compounds this problem, as lower testosterone levels combined with increased aromatase enzyme activity can create a perfect storm for gynecomastia development. Understanding how testosterone affects male breast tissue helps explain why some men benefit from testosterone therapy while others experience worsening symptoms.
Symptoms and Diagnosis of Gynecomastia

Recognizing the Signs of Gynecomastia
Gynecomastia is most commonly recognized by the development of glandular breast tissue in men, resulting in a noticeable enlargement of one or both breasts. Monitoring breast growth is important for diagnosing and understanding the progression of gynecomastia. This condition can cause discomfort, breast tenderness, and sometimes pain, especially when the area is touched. Some men may also experience increased nipple sensitivity or a feeling of fullness beneath the nipple. In many cases, the enlargement is uneven, with one breast appearing larger than the other.
How Gynecomastia Is Diagnosed
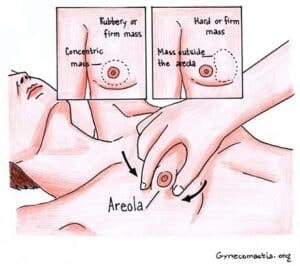
The first step in diagnosing gynecomastia is a thorough physical examination by a healthcare provider. During this exam, the doctor will assess whether the breast tissue is glandular—firm and rubbery—or primarily excess fatty tissue, which feels softer and more diffuse. Distinguishing between true gynecomastia (glandular tissue growth) and pseudogynecomastia (fat accumulation) is crucial, as the treatment approach may differ. The “pinch test” is used to determine the size of the breast tissue.
Because gynecomastia can sometimes mimic or mask more serious conditions like male breast cancer, your doctor will also look for warning signs, such as hard lumps, skin dimpling, or nipple discharge. If any of these are present, further evaluation is necessary to rule out breast cancer or other underlying issues.
To confirm the diagnosis and identify potential causes, your healthcare provider may order blood tests to check hormone levels, including testosterone and estrogen. Hormonal imbalances—such as low testosterone or elevated estrogen—are common contributors to the development of enlarged breast tissue. In some cases, additional tests may be needed to assess liver function, as liver disease can disrupt hormone metabolism and lead to gynecomastia. Imaging studies like mammography or ultrasound may also be recommended to distinguish glandular breast tissue from other abnormalities and exclude male breast cancer or cysts.

Understanding Causes and Treatment Options
Certain medications are known to cause gynecomastia as a side effect. These include anabolic steroids, anti androgens used for prostate conditions, and some calcium channel blockers prescribed for high blood pressure. If you are taking any of these medications and notice changes in your breast tissue, it’s important to discuss this with your doctor.
Gynecomastia can be classified into several types. Pubertal gynecomastia is common during adolescence and often resolves on its own. Puberty marks the second time gynecomastia can occur, affecting up to 60% of boys by age 14. Idiopathic gynecomastia refers to cases with no identifiable cause, while familial gynecomastia runs in families. Secondary gynecomastia can result from medical conditions such as liver disease, kidney failure, or hormonal disorders.
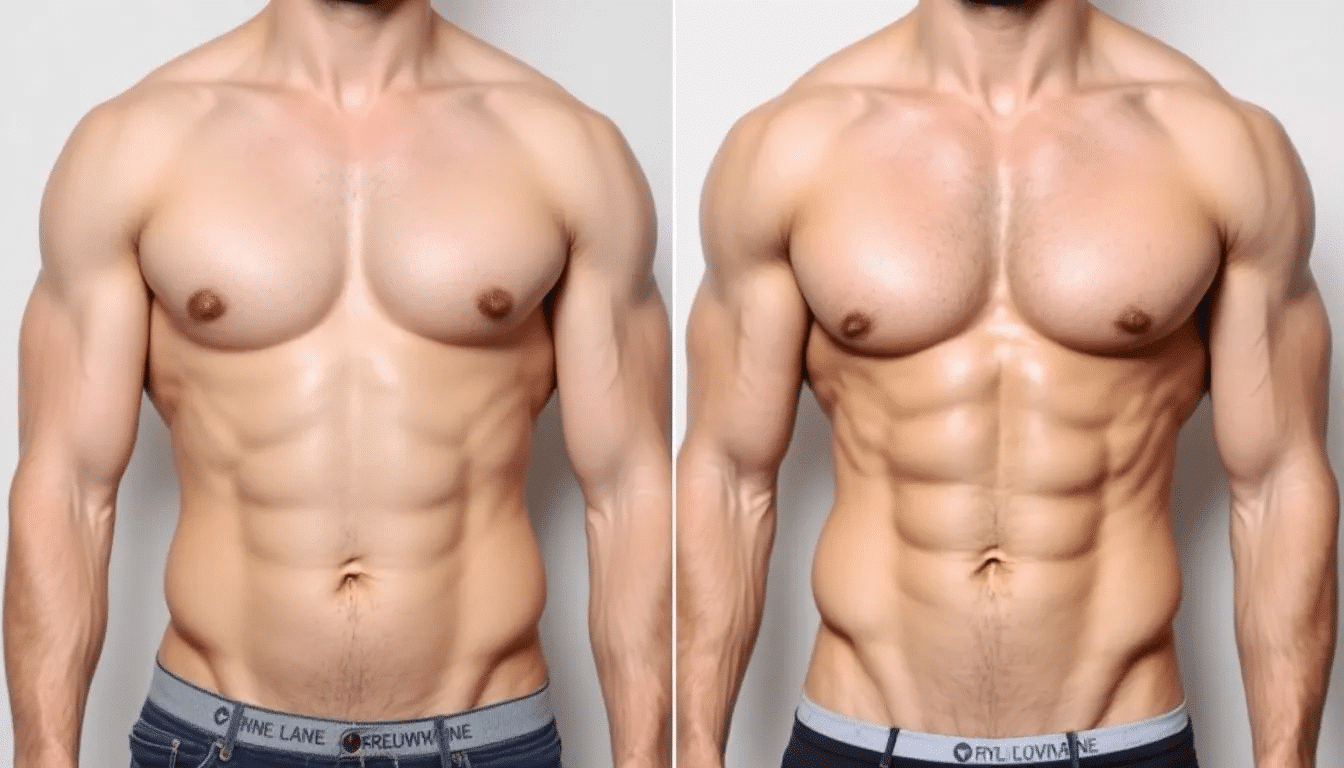
Treatment for gynecomastia depends on the underlying cause and severity of symptoms. In some cases, hormone replacement therapy—such as testosterone therapy—may be recommended to correct hormonal imbalances. If excess breast tissue persists or causes significant discomfort, surgical intervention may be considered for male breast reduction. Early diagnosis and treatment can help prevent long-term complications and improve quality of life.
While it’s not always possible to prevent gynecomastia, maintaining a healthy lifestyle, avoiding anabolic steroids and unnecessary medications, and managing underlying health conditions can help reduce your risk. If you notice any changes in your breast tissue, prompt medical evaluation is essential to determine the cause and develop an effective treatment plan tailored to your needs.
When Increasing Testosterone Helps Gynecomastia
When Testosterone Therapy Is Most Effective
Testosterone therapy is most beneficial for gynecomastia when the condition stems from genuine testosterone deficiency or hypogonadism. Men with primary hypogonadism, where the testes fail to produce adequate testosterone, often experience significant improvement in breast tissue enlargement when testosterone levels are restored to normal ranges through hormone replacement therapy. Emerging gynecomastia (new onset) is more likely to respond to TRT (testosterone replacement therapy) than long-standing cases where the tissue has become fibrous.
Klinefelter syndrome, a condition associated with primary hypogonadism, has a high prevalence of gynecomastia, occurring in about 80% of cases. Some tumors, like Leydig cell tumors, can cause gynecomastia by producing excess estrogen or increasing testosterone aromatized to estrogen.
Secondary hypogonadism, caused by pituitary gland dysfunction or pituitary insufficiency, represents another scenario where increasing testosterone can effectively treat gynecomastia. When the pituitary gland fails to stimulate adequate testosterone production, testosterone replacement therapy can help restore hormone balance and reduce male breast enlargement.
Certain medical conditions that cause testosterone levels to drop also respond well to testosterone therapy for gynecomastia treatment. These include Klinefelter syndrome, testicular tumors or testicular tumor complications, and androgen insensitivity syndromes. In these cases, addressing the underlying testosterone deficiency often leads to meaningful reduction in breast tissue growth.
Age-related testosterone decline can also contribute to gynecomastia development, particularly in older men who develop gynecomastia alongside other symptoms of low testosterone or Low-T. Many older men have developed gynecomastia due to these hormonal changes. When properly managed, testosterone replacement therapy in these individuals may help prevent further breast enlargement and potentially reduce existing glandular tissue if caught early enough.
Timing Matters for Treatment Success
The key factor determining success is timing. Men who develop gynecomastia due to low testosterone and seek treatment within the first 1-2 years have the best chances of seeing improvement with testosterone therapy. During this period, the breast tissue remains actively proliferative and more responsive to hormonal interventions. However, once gynecomastia has persisted for more than two years, it becomes less responsive to medical treatment and may require surgical intervention.
It is important to note that low testosterone can cause gynecomastia by reducing the suppression of breast tissue growth, allowing estrogen to promote its development.
When Testosterone Therapy Can Worsen Gynecomastia
Despite its potential benefits, testosterone therapy can worsen gynecomastia through aromatization, where excess testosterone converts to estradiol (a potent estrogen) via the aromatase enzyme. This conversion can lead to increased estrogen levels, which directly stimulate breast tissue growth and cause gynecomastia to worsen rather than improve. An elevated estrogen level can directly produce gynecomastia by stimulating the growth of glandular breast tissue in men.
Men who already have normal or elevated testosterone levels face the highest risk of worsening gynecomastia with testosterone therapy. Adding more testosterone when levels are already adequate increases the substrate available for aromatization, potentially leading to elevated estrogen levels and subsequent breast tissue proliferation. These hormonal changes can produce gynecomastia and lead to enlarged breasts in men undergoing testosterone therapy.
Certain risk factors increase the likelihood of testosterone-to-estrogen conversion and subsequent gynecomastia worsening. These include excess body fat (which contains high levels of aromatase enzyme), advanced age, genetic predisposition to high aromatase activity, and liver disease that affects hormone metabolism. Men with these risk factors may develop gynecomastia even with appropriately dosed testosterone therapy.
The misuse of anabolic steroids or supra-physiological testosterone doses significantly increases gynecomastia risk. Bodybuilders and athletes who use high-dose testosterone or anabolic steroids frequently develop gynecomastia due to excessive aromatization. This type of gynecomastia can be challenging to treat, and often requires both hormonal and surgical intervention.
The Aromatization Problem
The aromatase enzyme, found primarily in fat tissue, but also in skin, muscle, and other tissues, converts androgens like testosterone into estrogens. When testosterone levels increase through therapy or supplementation, more substrate becomes available for this conversion process, potentially leading to elevated estrogen levels despite higher testosterone.
Several factors influence aromatase enzyme activity and determine how much testosterone converts to estrogen. Obesity significantly increases aromatase activity, as adipose tissue is a major site of estrogen production. Men with higher body fat percentages are more likely to experience problematic estrogen conversion when using testosterone therapy. In these cases, men may overproduce estrogen due to increased aromatase activity, further increasing the risk of gynecomastia.
Age also affects aromatase activity, with older men typically showing increased conversion rates compared to younger individuals. This age-related increase in aromatization helps explain why some older men develop gynecomastia despite having adequate testosterone levels, and why testosterone therapy must be carefully managed in this population.
Genetic variations in aromatase enzyme expression create individual differences in testosterone-to-estrogen conversion rates. Some men naturally have higher aromatase activity and are more likely to develop gynecomastia when testosterone levels increase, regardless of their age or body composition.
Understanding the aromatization issue helps explain why some men develop gynecomastia even with high testosterone levels. It also shows why testosterone therapy alone may not be enough to treat the condition in every case. This knowledge has led to the development of combination treatment approaches that address both testosterone deficiency and excess estrogen production.
Optimizing Testosterone Therapy for Gynecomastia Treatment

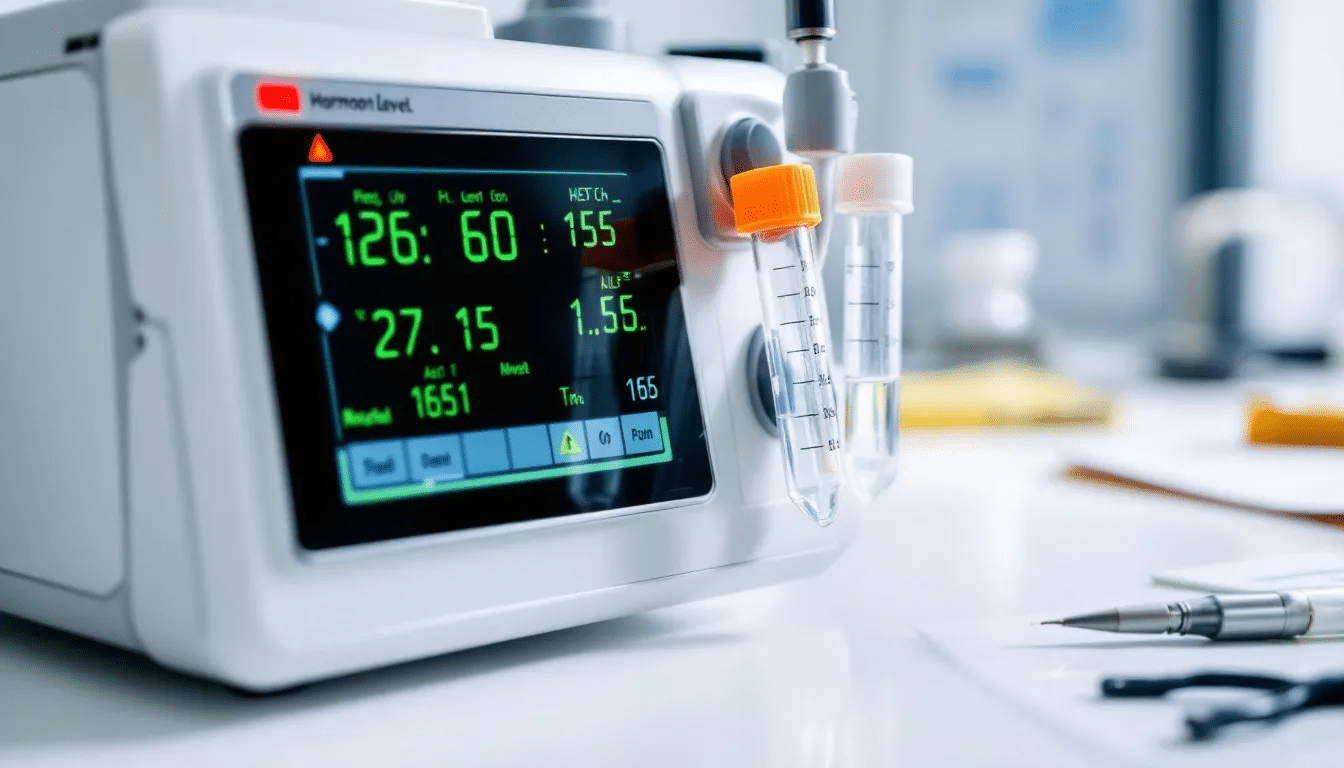
Successful testosterone therapy for gynecomastia requires comprehensive baseline hormone testing before starting treatment. Essential tests include total testosterone, free testosterone, estradiol, luteinizing hormone (LH), follicle-stimulating hormone (FSH), and prolactin levels. This baseline assessment helps determine whether testosterone deficiency actually causes the gynecomastia, and guides treatment planning. Identifying and correcting hormone imbalance is essential for effective gynecomastia treatment, as disturbances between estrogen and androgen levels can directly impact breast tissue development.
During testosterone replacement therapy, regular monitoring of both testosterone and estradiol levels is crucial for preventing gynecomastia worsening. Estradiol levels should be checked 4-6 weeks after starting therapy, and then periodically throughout treatment. If estradiol levels rise above optimal ranges, additional interventions may be necessary to prevent breast tissue growth. Regular monitoring of hormone levels during TRT is crucial to adjust dosages and prevent adverse effects, such as gynecomastia.
Aromatase inhibitors like anastrozole or letrozole can be used alongside testosterone therapy to prevent excess estrogen production. These medications block the aromatase enzyme, reducing the conversion of testosterone to estradiol and helping maintain optimal estrogen levels. However, aromatase inhibitors must be used carefully, as overly suppressing estrogen can cause other health problems.
Dosing strategies play a critical role in optimizing testosterone therapy for gynecomastia treatment. Lower, more frequent doses of testosterone often produce more stable hormone levels and less estrogen conversion compared to high, infrequent doses. Some men benefit from using testosterone gels or patches instead of injections to achieve more consistent hormone levels.
Combination Approaches
Combining testosterone with selective estrogen receptor modulators (SERMs) like Tamoxifen is one of the most effective approaches for treating gynecomastia. Tamoxifen blocks estrogen receptors in breast tissue, while testosterone therapy can address underlying hormone deficiency. Studies show Tamoxifen achieves complete or partial regression in 86-90% of gynecomastia cases. Tamoxifen has a higher success rate in resolving symptoms of gynecomastia than danazol based on study comparisons.
Raloxifene, another SERM, has shown particular promise in pubertal gynecomastia, with some studies reporting 91% efficacy rates. For adults with gynecomastia related to testosterone deficiency, combining raloxifene with carefully monitored testosterone therapy may provide superior results compared to either treatment alone.
The combination of testosterone replacement therapy with aromatase inhibitors can be particularly effective for men who develop gynecomastia despite normal testosterone levels. This approach addresses both potential testosterone deficiency and excess estrogen production, targeting multiple pathways involved in gynecomastia development.
Lifestyle modifications support optimal hormone balance and can enhance the effectiveness of testosterone therapy. Weight loss reduces aromatase enzyme activity in fat tissue, potentially decreasing estrogen production. Regular resistance training helps maintain muscle mass and may support healthy testosterone levels naturally.
Timeline considerations are important when implementing combination approaches. Most patients begin to see improvement within 3-6 months if the treatment approach is appropriate for their specific case. However, maximum benefits may not occur until 12-18 months of consistent therapy, and some chronic cases may require surgical consultation despite hormonal interventions. Gynecomastia that doesn’t improve with medical treatment often needs a surgical consultation for proper management.
Factors That Influence Treatment Success
The duration of gynecomastia before treatment significantly impacts the likelihood of success with testosterone therapy. Acute gynecomastia, present for less than 12 months, is more likely to respond to hormonal interventions compared to chronic gynecomastia, which has been present for years. Early intervention provides the best opportunity for meaningful breast tissue reduction.
The degree of fibrous tissue formation in the breast area determines responsiveness to hormone therapy. Fresh glandular breast tissue responds better to testosterone therapy and anti-estrogen treatments, while established fibrous tissue rarely shrinks with hormonal interventions alone. Physical examination and sometimes imaging studies can help assess tissue composition. Treatments like liposuction only remove fat and do not address the breast gland tissue. Surgery, such as mastectomy, may be necessary to remove the actual breast gland tissue.
A patient’s age can affect how well treatment works. Younger men usually have breast tissue that responds better and more balanced hormone metabolism, so they often benefit more from testosterone therapy. Older men may have more fibrous tissue and higher aromatase activity, which can make treatment harder and may require a more aggressive, combined approach.
The presence of underlying medical conditions affects treatment outcomes. Men with liver disease, kidney failure, or other chronic conditions may have altered hormone metabolism that impacts treatment effectiveness. Certain medications, including calcium channel blockers and anti androgens, can interfere with hormone therapy and may need adjustment during treatment. Painful gynecomastia may indicate active tissue growth or inflammation, and can influence the choice of treatment.
Individual hormone metabolism patterns vary significantly between patients and strongly influence treatment success. Men with naturally high aromatase activity may require aromatase inhibitor therapy regardless of their testosterone levels, while those with low aromatase activity may benefit from testosterone therapy alone.
Treatment Options
Non-Surgical Treatment Alternatives
When testosterone therapy alone proves insufficient for treating gynecomastia, several alternative approaches can provide additional benefits. Selective estrogen receptor modulators like tamoxifen and raloxifene have shown excellent results for reducing breast tissue enlargement, with tamoxifen demonstrating strong evidence for gynecomastia treatment.
Aromatase inhibitor therapy can be effective for men whose gynecomastia results from excess estrogen production, rather than testosterone deficiency. Medications like anastrozole help reduce estrogen levels by blocking the conversion of testosterone to estradiol, addressing one of the primary drivers of breast tissue growth.
Natural testosterone boosters have limited evidence for treating gynecomastia, but may provide modest benefits as part of a comprehensive approach. Compounds like D-aspartic acid, zinc, and vitamin D can support healthy testosterone production, though they’re unlikely to produce dramatic improvements in established gynecomastia cases.
Lifestyle interventions play a crucial role in gynecomastia treatment. Weight loss reduces aromatase enzyme activity in adipose tissue, potentially decreasing estrogen production and improving hormone balance. Regular exercise, particularly resistance training, can help maintain muscle mass and support healthy testosterone levels naturally.
Dietary modifications may help optimize hormone balance and support gynecomastia treatment. Reducing processed foods, limiting alcohol consumption, and including foods rich in zinc and vitamin D can support healthy testosterone production. However, dietary changes alone are rarely sufficient for treating established gynecomastia. Liver failure can disrupt hormone metabolism, leading to increased estrogen levels and contributing to the development of gynecomastia, especially in individuals with cirrhosis or alcoholic liver disease.
When Surgery Becomes the Best Option
When medical treatments fail to provide satisfactory results, gynecomastia surgery becomes the most definitive treatment option. Surgical procedures range from liposuction for cases with significant fat tissue to mastectomy techniques for removing glandular tissue. Liposuction is particularly effective for removing excess fat deposits in the chest, but it does not address glandular breast tissue. Surgical intervention may be warranted if gynecomastia is severe or results in significant psychological distress. Male breast reduction surgery offers the highest success rates for men with chronic gynecomastia or those who don’t respond to hormonal interventions.
Psychosocial Impact of Gynecomastia
Studies suggest that gynecomastia may be associated with depression in some men. The embarrassment associated with gynecomastia can hinder a man’s social interactions. Some men may develop eating disorders as a response to body image issues related to gynecomastia. Support groups exist to help men manage the emotional impact of gynecomastia.
Monitoring and Safety Considerations
Regular blood work is essential during testosterone therapy to ensure safe and effective treatment. Initial monitoring should include testosterone levels, estradiol, complete blood count, liver function tests, and prostate-specific antigen (PSA) levels. Follow-up testing typically occurs at 3-month intervals initially, then every 6 months once stable levels are achieved.
Recognizing signs that testosterone therapy is worsening gynecomastia helps prevent progression and allows for treatment modifications. Warning signs include increased breast tenderness, visible enlargement of one or both breasts, nipple sensitivity, or new onset of breast pain. Any of these symptoms warrant immediate medical evaluation and potential treatment adjustment. Men with advanced prostate cancer often receive androgen deprivation therapy, which can lead to gynecomastia as a side effect.
Potential side effects of testosterone therapy extend beyond gynecomastia concerns and require ongoing monitoring. These may include sleep apnea worsening, increased red blood cell count, mood changes, and potential cardiovascular effects. Men with a history of prostate cancer or breast cancer should avoid testosterone therapy due to safety concerns.
Contraindications for testosterone therapy include active prostate cancer, male breast cancer, untreated sleep apnea, and severe heart failure. Men with these conditions should not use testosterone therapy and should explore alternative treatments for gynecomastia. Additionally, androgen deprivation therapy for advanced prostate cancer can lead to male breasts due to hormonal changes. Men trying to father children should be aware that testosterone therapy can suppress sperm production.
Proper dosing and administration help minimize side effects while maximizing benefits. Starting with lower doses and gradually increasing based on response and side effects provides the safest approach. Different testosterone preparations (injections, gels, patches) have varying risk profiles, and the choice should be individualized based on patient factors and preferences.
When to Adjust or Stop Testosterone Therapy
When to discontinue or modify testosterone therapy depends on treatment response and side effect development. Men who develop worsening gynecomastia, significant side effects, or achieve their treatment goals may need therapy adjustments. Some men may benefit from cycling testosterone therapy or switching to alternative treatments.
Long-term Outlook and Expectations
Realistic timeframes for improvement with testosterone therapy usually range from 3 to 6 months for initial changes. Maximum benefits are often seen between 12 and 18 months. Men with acute gynecomastia caused by testosterone deficiency tend to see the most dramatic improvements. Those with chronic gynecomastia may notice more modest changes.
Several factors can predict treatment success. These include younger age, recent onset of gynecomastia, confirmed testosterone deficiency, minimal fibrous tissue development, and low aromatase activity. Men who meet these criteria have the highest likelihood of meaningful breast tissue reduction with testosterone therapy.
Maintenance therapy requirements vary based on the underlying cause of testosterone deficiency. Men with permanent hypogonadism typically require lifelong testosterone replacement therapy to maintain results and prevent gynecomastia recurrence. Those with temporary causes may discontinue therapy once the underlying issue resolves. However, it is important to note that certain medications or medical conditions can produce gynecomastia even after initial treatment success, especially if they increase estrogen levels or disrupt androgen production.
Long-term hormone optimization often requires ongoing adjustments based on aging, weight changes, and other factors that affect hormone metabolism. Regular monitoring and treatment modifications help maintain optimal results while minimizing side effects. Some men may benefit from periodic breaks in therapy to assess natural hormone recovery.
When surgical consultation should be considered, it depends on treatment response and patient goals. Men who don’t achieve satisfactory results within 12-18 months of optimal medical therapy may benefit from surgical evaluation. Additionally, those with significant fibrous tissue formation or cosmetic concerns may prefer surgical intervention for more predictable results.
The combination of medical and surgical approaches sometimes provides the best long-term outcomes. Some men benefit from hormonal optimization before surgery to minimize recurrence risk, while others may use hormone therapy to maintain results after surgical intervention.
Consultation with Dr. Delgado
Dr. Delgado offers both virtual and in-person consultations. To schedule an appointment, please call 415-898-4161.
Frequently Asked Questions
How long does testosterone therapy take to reduce gynecomastia?
Improvement typically begins within 3-6 months if testosterone therapy is effective for the individual case. Maximum benefits usually occur within 12-18 months of consistent treatment. Early-stage gynecomastia responds faster than chronic cases with established fibrous tissue. Some men may notice initial worsening before improvement due to hormone fluctuations during the adjustment period.
Can I use testosterone therapy if I already have normal testosterone levels?
Testosterone therapy is generally not recommended for men with normal testosterone levels. Adding testosterone when levels are already adequate increases the risk of aromatization and worsening gynecomastia. Alternative treatments like SERMs or aromatase inhibitors may be more appropriate. Comprehensive hormone evaluation should guide treatment decisions, rather than testosterone levels alone. TRT is not recommended for men with normal testosterone levels, as it can have negative effects.
What are the warning signs that testosterone therapy is making gynecomastia worse?
Increased breast tenderness or sensitivity within the first few weeks of treatment indicates potential worsening. Visible enlargement of breast tissue or nipple changes require immediate medical attention. Elevated estradiol levels on follow-up blood work suggest problematic estrogen conversion. New onset of breast pain or discomfort that wasn’t present before therapy should prompt treatment evaluation and potential modification.
Should I combine testosterone with aromatase inhibitors from the start?
This decision depends on individual risk factors, including body weight, age, and baseline estradiol levels. Men with higher aromatase activity may benefit from prophylactic aromatase inhibitor use. Starting with testosterone alone allows assessment of individual response before adding additional medications. Close monitoring during initial weeks can guide decisions about combination therapy based on hormone level changes.
Is gynecomastia reversal permanent once achieved with hormone therapy?
Reversal of glandular tissue through hormone therapy can be permanent if underlying causes are addressed. Continued hormone optimization is usually necessary to maintain results and prevent recurrence. Weight gain, medication changes, or aging can potentially cause gynecomastia to return. Fibrous tissue that has already formed may not fully reverse with hormone therapy alone and may require surgical intervention for complete correction.
Weight Gain and Gynecomastia
Weight gain is a significant factor in the development and progression of gynecomastia. When men carry excess body fat, especially around the chest and abdomen, their fat tissue becomes more hormonally active. This increase in fat triggers higher production of the aromatase enzyme. Aromatase is responsible for converting testosterone into estrogen, which can lead to increased estrogen production in the body. Elevated estrogen levels can stimulate breast tissue growth. As a result, men who are overweight or obese are more likely to develop gynecomastia or see existing symptoms worsen.
As body fat increases, the risk of developing gynecomastia also rises. More fat tissue leads to greater aromatase activity, which raises estrogen levels. This hormonal shift can cause visible breast tissue growth, making the condition more noticeable and harder to treat. Maintaining a healthy weight through a balanced diet and regular exercise is key to lowering the risk of gynecomastia. It also helps manage existing symptoms. Keeping body fat under control supports healthy estrogen levels and overall hormone balance. This is important for preventing unwanted breast tissue development.
Lifestyle Changes for Gynecomastia
Adopting healthy lifestyle habits can make a meaningful difference in both preventing and managing gynecomastia. One of the most effective steps is to maintain a healthy weight, as excess body fat increases the risk of developing gynecomastia by promoting higher estrogen levels. Incorporating regular exercise, such as cardiovascular workouts and strength training, helps reduce body fat and supports healthy hormone levels.
A nutritious diet is also key. Focus on eating plenty of fruits, vegetables, whole grains, and lean proteins, while limiting saturated fats and processed foods. These dietary choices can help regulate hormone levels and reduce the likelihood of developing gynecomastia. It’s equally important to avoid substances that can disrupt hormone balance, such as anabolic steroids, which are known to increase the risk of gynecomastia by altering testosterone and estrogen levels.
Other beneficial lifestyle changes include getting enough sleep, managing stress, and avoiding excessive alcohol consumption. Chronic stress and poor sleep can negatively impact hormone production, further increasing the risk of developing gynecomastia. By making these positive changes, men can support healthy hormone levels, reduce body fat, and lower their chances of experiencing unwanted breast tissue growth.
Breast Cancer Risk in Men with Gynecomastia
Although gynecomastia itself does not directly cause breast cancer, men with this condition may have a slightly higher risk of developing breast cancer due to underlying hormonal imbalances. The presence of enlarged breast tissue can sometimes be a sign that estrogen levels are elevated or that there is another hormonal imbalance at play, both of which can increase the risk of breast cancer in men.
It’s important for men with gynecomastia to be vigilant about changes in their breast tissue. Warning signs of male breast cancer include the development of a hard lump, thickening in the breast tissue, changes in the skin or nipple, or unusual discharge. If any of these symptoms are noticed, prompt medical evaluation is essential. Regular check-ups with a healthcare provider can help monitor breast tissue health and catch any potential issues early, reducing the risk of breast cancer and ensuring timely treatment if needed. By staying informed and proactive, men with gynecomastia can protect their health and address any concerns related to breast cancer risk.
